BCG vaccination for TB – an investigative journey
Intro
Not to be difficult, but recently a few questions about the BCG vaccine for tuberculosis (TB) have been bothering me. I keep hearing it stated that when it comes to interpreting the tuberculosis skin test (TST), BCG vaccination status doesn’t matter – a positive test should be treated as latent disease. Fine, that’s the
policy. Does it really make sense, though? Since we know that BCG vaccination causes a positive TST, it seems a little strange. Additionally, why the dismissive language? I mean, clearly BCG vaccination status does matter – it means that if your skin test is positive, even if we are going to treat you for TB, you probably don’t have the disease. I hope we aren’t just being vindictive in trying to show other countries that not only do we disagree with BCG vaccination, but we feel strongly enough about it to make BCG vaccinated immigrants undergo a full course of unneeded TB treatment.
Background
To investigate this matter, let’s first look at the big picture. According to the
World Health Organization (WHO), tuberculosis:
-- exists as a latent infection in one third of the world’s population (2.23 billion people)
-- causes 14.6 million active infections
-- causes 8.9 million new active cases yearly
-- causes 1.7 million deaths yearly
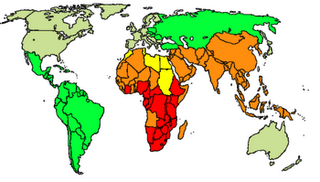
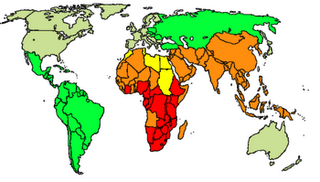
World TB incidence. Cases per 100,000; Red = >300, orange = 200-300; yellow = 100-200; green 50-100 and grey <50. (
Wikipedia)
The vaccine
The vaccine in question is an attenuated live vaccine (Bacillus of Calmette and Guerin) prepared originally from Mycobacterium bovis (a sister bug of Mycobacterium tuberculosis) in 1921 but that now exists as a variety of strains. It is of variable effectiveness, and the particular strain used may be important, but it seems to be about 50% effective in preventing active pulmonary tuberculosis and 85% effective in preventing disseminated or meningeal TB, the worst kind
1. This is comparable to the protection given by treating latent TB, which was shown to be between 25 and 93% in studies done in the 1950s and 60s
1. The vaccine’s ability to prevent childhood tubercular meningitis, in fact, is one of the primary justifications for its administration.
Over 100 countries currently have universal childhood vaccination policies, including Japan, Finland, Portugal, Ireland, and Poland. In the U.S., we have never had a universal childhood vaccination, mostly because tuberculosis is somewhat rare in the U.S., vaccination is only of limited effectiveness, and because the vaccine interferes with the TST. Current
CDC guidelines in fact recommend considering BCG vaccination only in two very rare situations: when children with negative skin tests are living with actively infected adults who are untreated, ineffectively treated, or have multi-drug resistant strains of TB, and when health care workers are working in high incidence settings where TB control precautions have failed and there is ongoing transmission of TB to health care workers.
The problem
The problem with BCG vaccination and the TST is that 90% of people will have a positive skin test within 8 weeks of receiving the vaccine, but only 20% will still have a positive skin test after 10 years
1. Therefore, if someone is five years out and has a positive skin test, it’s unclear whether the positive result is because of BCG or because of actual latent disease. In the U.S. we treat these people for latent TB even though there is no evidence that treating in this case is actually beneficial.
The solution
So why don’t we have a better TB test that can tell the difference between latent TB infection and BCG vaccination? Well, now we do. It’s called
serum interferon gamma testing, it was approved by the FDA in 2005, and it detects tuberculosis as well as the skin test without being affected by BCG vaccination status. There’s no longer a reason to treat people for TB unless they actually have it.
The UK Experience
The UK was universally vaccinating school children until 2005, but at that time it decided the prevalence of TB was no longer high enough to justify routine vaccination. Instead, it adapted a
policy of offering the BCG vaccine to high risk children, which it defined as children who:
–live in areas where the incidence of TB is >40/100,000
–live with parents from a country where the prevalence is >40/100,000
–themselves are new unvaccinated immigrants from countries with a high TB rate
This type of program is typical of European countries. The International Union Against Tuberculosis and Lung Disease actually offers guidelines to nations regarding universal vaccination policies, and when they may safely be discontinued
2. Currently, they state that when the TB incidence rate falls below 15/100,000, it is safe for countries to discontinue universal vaccination.
TB in the U.S.
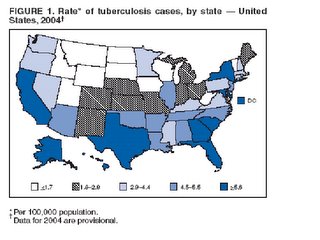
The U.S. currently has a rate well below that threshold; in 2004,
U.S. incidence of active TB reached an all-time low of 4.9/100,000, down from 52.6/100,000 in 1952. In
DC, however, the rate is much higher, most recently 12-15/100,000 in 1999-2000. (I was unable to find more current data.) If you exclude the Northwest quadrant of the city, that rate would clearly be much higher yet. Considering that we do have pockets of high TB incidence like DC in the U.S., switching to a European-style policy of offering vaccination to high risk children may make good sense.
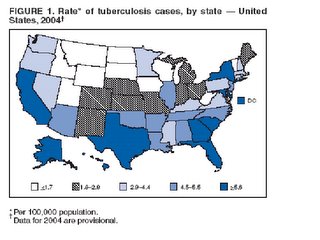
(Source:
CDC)
An Aussie Idea
A recent
paper in the Medical Journal of Australia suggested offering BCG vaccination to Australian medical students. They noted that although the Australian incidence of TB is low, Australian medical students like to perform foreign electives in areas of high TB prevalence, where having been vaccinated would benefit them.
A Few Conclusions
BCG isn’t a great vaccine, but it does provide an intermediate level of protection against TB, and it appears to be about equally effective as the treatment of latent disease once somebody has been infected. In this new era of serum interferon gamma, although cost may be an issue, TST interference is no longer a reason to withhold vaccination. BCG vaccination status matters, and we no longer need to treat our BCG vaccinated patients with positive TSTs if their interferon gamma is negative. As for the rest of the U.S. policy, it may be time for some revision.
Adapting a European-style vaccination model of offering vaccination to those children at highest risk for TB could selectively protect the children who need it without compromising our current methods of diagnosis, treatment, control, and prevention.
References (direct links provided to the others):
1Glassroth, Jeffrey and Christopher Crnich. Tuberculosis in Baum’s Textbook of Pulmonary Diseases. 7th ed. Lippincott Williams and Wilkins:2004.
2Criteria for discontinuation of vaccination programmes using Bacille Calmette-Guérin (BCG) in countries with a low prevalence of tuberculosis. A statement of the International Union Against Tuberculosis and Lung Disease. Tuber Lung Dis 1994;75(3):179-80
There's a study for everything
Like its religious counterparts the Bible and the Koran, both notorious for providing great interpretive flexibility in their guidance of moral human behavior, the medical literature also, while providing a framework for best medical practice, leaves plenty of space for, well, the
art of medicine. The Bible and the Koran are well known for passages that have been used to rationalize slavery, violence, and hatred, even while their over-riding themes teach against these practices. In the medical literature, similarly, if you are willing to dig a little bit (and extrapolate to a reasonable extent), there is in fact a study for everything. If you want to prove that eating red clover slows down aging, there’s a
study to back you up. Conversely, if your point is to show that red clover is actually toxic, well, you’ll find
that too. What’s important is not the details of the particular study, but your ability to spout it off quickly and confidently. Because evidence (the noblest form of which is the randomized controlled trial) occupies such an exalted place in medicine, beyond the reproach of common practice, logic, physiology, sensibility, or any other possible objections of the mere human mind, one good study in your pocket is all you need to justify pretty much anything you wish to do. In fact, the more obscure your study, the better, as nobody will be able to challenge a study that they haven’t read.
Pharmaceutical companies and representatives are well acquainted with the power and the flexibility of studies. It’s a simple numbers game actually: if aspirin and plavix, for example, work equally well in stroke prevention, and you run the study comparing them twenty times, requiring 95% confidence for a positive conclusion, on average one out of those twenty studies will show that plavix works better. Eureka! You can discard the other nineteen studies, since, as already mentioned, all you really need is one.
Medicine does have a defense against the capriciousness of individual studies, though; it’s called the meta-analysis. In a meta-analysis, you collect all of the studies you can find on a subject, pool them together, and determine the overall result. Unfortunately, even meta-analyses don’t always agree with each other. Case in point, my
review of pseudomonas double coverage last month: a meta-analysis of 17 studies by
Safdar et al. in 2004 showed that antibiotic double coverage of pseudomonas bacteremias decreases mortality by half, while a meta-analysis of 64 studies by
Paul et al. in 2006 showed no benefit to double coverage. What we need is a meta-meta-analysis. A supercalifragilistic-expialidocious-alysis.
Of course, there aren’t any studies when it comes to doing things that actually make sense. The study, for example, to determine if
parachutes reduce mortality in sky diving, has never been done. Crazy ideas, like making residents
go home after 30-hour shifts instead of finishing out their work days post-call—those are the only ones that need studies. For that reason, the next time that somebody quotes a study to you, be advised that whatever it is they’re proposing, it’s probably nuts. After all, if you need a study to justify something, it means it already failed the test of common sense.
A harp in the hospital
As much as I love classical music, I’ve never really appreciated the harp. Give me the violin with its impassioned cry, the piano with its majestic voice, the cello with its silky song, the oboe with its saccharine sweetness, but the harp? I know it’s the instrument of angels, but it reminds me more of the harpsichord, that plucky and clumsy instrument people used to play before they invented the piano.
A harp in the hospital, though, is an entirely different matter. Imagine yourself standing there on rounds, concentrating on the patient presentation but also thinking about getting to morning report on time, about rushing off to clinic, about the dozens of discharge summaries that are building up, and then from out of nowhere you hear these soft, beautiful, arpeggiated chords, each pluck of string producing a perfectly round bead of music that courses through your body and just dissipates any and all stress. A run of six notes, then eight, then twelve, and the tension that you didn’t even realize you were carrying magically resolves; it effortlessly dissolves. You look around for the source of this miracle, and there she is, a pepper-haired, gentle-faced, middle-aged woman, ever so slowly making her way down the corridor, spreading her music by letting it float out in concentric circles from her golden harp. Your heart cries out, “Linger! Stay near us just a minute more! For although we are not patients here, we also need your healing!” And she does, for a second, but then she continues on, as there are more who need the gift of her song. Back to rounds—actually, the patient presentation never stopped, but now it is somehow more bearable, a bit more important even? I wonder, does she think because we are doctors that we don’t believe in the healing power of her music?
The doctor card continued. . .techniques of disclosure
Before continuing, please make sure you have read the
intro and Part I.
Part II. Techniques of disclosure
These techniques are really only practical in one situation: when you need a little extra help with your dating game and don’t mind humiliating yourself to get it.
1. Direct and shameless:
”Hi, I’m not sure we’ve met. I’m Sara.”
“Hi, I’m Doctor Adam Miller.”
It’s all in the intro. For those a little less brazen, this could be softened by “Whoa, I can’t believe that just slipped out. . . I’ve been spending WAY too much time in the hospital!”
2. That reminds me:
”Oh, so you’ve recently been traveling in Germany? That reminds me of this German patient I have in clinic who has just the largest nose. . .”
Rather flexible and simple—very useful!
3. The concerned patient:
Step 1: Set your cell phone to go off after 3 minutes.
Step 2: Initiate conversation with the person of choice.
Step 3: When the phone rings, excuse yourself but audibly begin the following script:
“Mr. Johnson?. . .No, it’s quite all right for you to call me on my private line. . .your epigastric pain is still bothering you? I want you to go ahead and double the dose of the protonix you are on. . .that’s right, I think you will be feeling better soon. I’ll see you in clinic next week. . .you’re welcome, good-bye. . .[returning your attention to your conversation partner] . . .Sorry about that. So you were telling me about the local beaches?”
Beware, this technique can be associated with feelings of guilt, and if it fails, you may find yourself sunken to a new low.
4. The business card:
Your most beloved and trusted friend.
5. The location slip:
”I was just leaving the hospital where I work today, and I saw the strangest thing. . .there was a rainbow in the sky, but it was in black and white. . .”
Amazing things can happen on one’s way to and from the hospital.
6. DOC or MD plates:
You’ve seen them. Don’t knock it until you’ve tried it.
7. Heimlich this:
Step 1: Pay your buddy five bucks.
Step 2: Enter into conversation with a desired party.
Step 3: Signal your buddy, who then begins to loudly and dramatically choke on an olive.
Step 4: Rush over behind him and quickly deliver three epigastric thrusts, the last of which should dislodge the offending olive.
Step 5: Nonchalantly return to conversation with the desired party.
Don’t inform your buddy, but make sure you choose a bar that’s within five minutes of a hospital, just in case the olive decides to play tough guy.
8. Scrubbing it:
Don’t be afraid to show your working blues. Some tips on how to maximize their impact:
1. For added credibility, the more scrub-clad group members, the better
2. More effective at happy hour than on Saturday night
3. Good hygiene is important, but if you are freshly showered and clean shaven, it does raise the question of why you didn’t get a chance to throw on some real clothes.
4. Try khaki bottoms for a hip and more seasoned look
9. The teetotaler:
“Yeah, I’m sticking to the non-alcoholic stuff tonight—I’m on call for the hospital and could have to go cover at a moment’s notice.”
Mysterious and exciting, yet responsible. . .that’s hot!
Final thought:
Armed with these methods, you should be able to reveal or conceal your M.D. status as you choose. Some of them are rather simple to employ, but others require considerable practice, nuance, and planning. Don’t be afraid to put in the necessary work. Getting into medical school wasn’t easy, and neither is becoming a skilled socialite. Whether the goal is to avoid the curious inquiries of over-eager onlookers or to win the heart of that very special person, the payoff may be greater than you think.
The doctor card
My brothers believe it’s the ultimate trump card, that all I have to do in casual conversation with a woman to win her over is to somehow slip in the information that I’m a medical doctor. Every woman, they believe, is yearning, aching even, to be with a doctor, and the moment I reveal my profession, nothing more need be said. I can simply sit back and let the title do its work.
Stated in general terms, medicine is perceived to be a noble, prestigious, and well paying profession, and its practitioners are thought to be intelligent, dedicated, and compassionate. Yeah, as residents we know it, being a doctor is sexy.
Most of the time, though, we’d rather not play the doctor card; we’d prefer to just fit in. Although we’re privately proud of the hard work that turned us into doctors, we don’t want to flaunt it or flash it in anyone’s face. In DC, where one’s profession comes up early and often in polite conversation, being able to handle the topic tastefully is a particularly useful skill. But how do we reveal our profession graciously without attracting unwanted attention? Is there a way to subtly change the topic and avoid revelation at all? Additionally, for those times when we do want to tap into the prestige of being a doctor, how do we so tactfully?
Coming up with a good strategy for when and how to play the doctor card, and when and how to withhold it, is key to resident survival. In the following guide I humbly introduce and comment on the effective use of several conversational techniques that I have found to be especially useful.
Part I. Techniques of obscuration
These techniques are practical in a variety of situations, but are intended for social settings where downplaying your status as medical doctor/resident may be appropriate. This includes, but is not limited to, situations where:
--your conversation partner has just announced that he/she is newly unemployed
--ten minutes ago a bystander collapsed and you innocently looked on, feigning non-interest
--you’re having difficulty getting out more than a few words at a time because of the four cigars you have stuffed in your mouth
--the rest of the group is laughing about the idiot doctor they just nailed in malpractice court
--you just stiffed your waiter to save a buck
--a smallpox outbreak was just discovered at your hospital
--you were unable to come up with the answer when somebody casually asked, “What’s in Nyquil, anyway?”
--for once you are actually feeling confident enough to get the girl/guy on your own merit
1. Perpetual vagueness:
“So what brought you to DC?”
“Work.”
“Where do you work?”
“At Georgetown.”
“Do you teach there?”
“No.”
“So what do you do?”
“I work at the hospital.”
“And what do you do at the hospital?”
“I take care of patients.”
“Ok, so you’re a nurse?”
“Uh, something like that.”
Most people will take the hint after the 2nd or 3rd question, and you’ll rarely be pressed to the bitter end. The danger of this technique is that it is known to cause extreme irritation in the opposing party.
2. The spy con:
“What do you do?”
“I work for the government.”
“What type of work?”
“You know, one of those jobs where it’s best not to get into the specifics.”
Since Medicare pays for us, not technically a lie. This technique works best in Washington; in other locations (particularly Red states) people will just think you’re unemployed.
3. Technical jargon:
“What do you do?”
“I’m a house officer performing an elective rotation in electrophysiology. How about you?”
“Say what?”
The more specific, the better.
4. No English:
“What do you do?”
“No English, no English.”
Harder to pull off if you're white.
5. The intern deception:
“What do you do?”
“I’m an intern.”
“Oh really, where?”
“One of the companies in Foggy Bottom.”
“How’s that going?”
“Not bad, not bad.”
“Oh, that reminds me, I have a problem maybe you could help me with. My wife keeps giving me crap about the coffee I make . . .any suggestions on how to keep it tasting fresh?”
“Good one.”
6. The sleight of ear:
“What do you do?”
“What do I think of the zoo? Oh, aren’t the pandas just wonderful?”
Works well in chain sequence. (i.e. “No, I asked what do you do?”. . .“What? There’s something on my shoe? Good heavens!”. . .)
7. The counter attack:
“What do you do?”
“Nice try, asshole. You’re probably some hotshot doctor or lawyer asking me what I do just so I’ll return the question and you’ll be able to show off your impressive job. When’s the last time a janitor asked ‘what do you do?’”
Not recommended for use against women.
8. The beast within:
“What do you do?”
“Excuse me, nature calls.”
Coming soon:
Part II
Techniques of disclosure