BCG vaccination for TB – an investigative journey
IntroNot to be difficult, but recently a few questions about the BCG vaccine for tuberculosis (TB) have been bothering me. I keep hearing it stated that when it comes to interpreting the tuberculosis skin test (TST), BCG vaccination status doesn’t matter – a positive test should be treated as latent disease. Fine, that’s the policy. Does it really make sense, though? Since we know that BCG vaccination causes a positive TST, it seems a little strange. Additionally, why the dismissive language? I mean, clearly BCG vaccination status does matter – it means that if your skin test is positive, even if we are going to treat you for TB, you probably don’t have the disease. I hope we aren’t just being vindictive in trying to show other countries that not only do we disagree with BCG vaccination, but we feel strongly enough about it to make BCG vaccinated immigrants undergo a full course of unneeded TB treatment.
Background
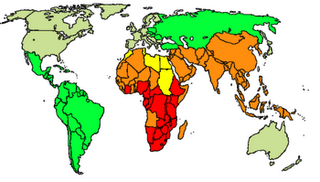
To investigate this matter, let’s first look at the big picture. According to the World Health Organization (WHO), tuberculosis:
-- exists as a latent infection in one third of the world’s population (2.23 billion people)
-- causes 14.6 million active infections
-- causes 8.9 million new active cases yearly
-- causes 1.7 million deaths yearly
World TB incidence. Cases per 100,000; Red = >300, orange = 200-300; yellow = 100-200; green 50-100 and grey <50. (Wikipedia)
The vaccine
The vaccine in question is an attenuated live vaccine (Bacillus of Calmette and Guerin) prepared originally from Mycobacterium bovis (a sister bug of Mycobacterium tuberculosis) in 1921 but that now exists as a variety of strains. It is of variable effectiveness, and the particular strain used may be important, but it seems to be about 50% effective in preventing active pulmonary tuberculosis and 85% effective in preventing disseminated or meningeal TB, the worst kind1. This is comparable to the protection given by treating latent TB, which was shown to be between 25 and 93% in studies done in the 1950s and 60s1. The vaccine’s ability to prevent childhood tubercular meningitis, in fact, is one of the primary justifications for its administration.
Over 100 countries currently have universal childhood vaccination policies, including Japan, Finland, Portugal, Ireland, and Poland. In the U.S., we have never had a universal childhood vaccination, mostly because tuberculosis is somewhat rare in the U.S., vaccination is only of limited effectiveness, and because the vaccine interferes with the TST. Current CDC guidelines in fact recommend considering BCG vaccination only in two very rare situations: when children with negative skin tests are living with actively infected adults who are untreated, ineffectively treated, or have multi-drug resistant strains of TB, and when health care workers are working in high incidence settings where TB control precautions have failed and there is ongoing transmission of TB to health care workers.
The problem
The problem with BCG vaccination and the TST is that 90% of people will have a positive skin test within 8 weeks of receiving the vaccine, but only 20% will still have a positive skin test after 10 years1. Therefore, if someone is five years out and has a positive skin test, it’s unclear whether the positive result is because of BCG or because of actual latent disease. In the U.S. we treat these people for latent TB even though there is no evidence that treating in this case is actually beneficial.
The solution
So why don’t we have a better TB test that can tell the difference between latent TB infection and BCG vaccination? Well, now we do. It’s called serum interferon gamma testing, it was approved by the FDA in 2005, and it detects tuberculosis as well as the skin test without being affected by BCG vaccination status. There’s no longer a reason to treat people for TB unless they actually have it.
The UK Experience
The UK was universally vaccinating school children until 2005, but at that time it decided the prevalence of TB was no longer high enough to justify routine vaccination. Instead, it adapted a policy of offering the BCG vaccine to high risk children, which it defined as children who:
–live in areas where the incidence of TB is >40/100,000
–live with parents from a country where the prevalence is >40/100,000
–themselves are new unvaccinated immigrants from countries with a high TB rate
This type of program is typical of European countries. The International Union Against Tuberculosis and Lung Disease actually offers guidelines to nations regarding universal vaccination policies, and when they may safely be discontinued2. Currently, they state that when the TB incidence rate falls below 15/100,000, it is safe for countries to discontinue universal vaccination.
TB in the U.S.
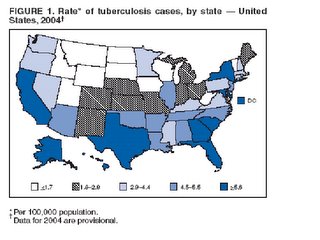
The U.S. currently has a rate well below that threshold; in 2004, U.S. incidence of active TB reached an all-time low of 4.9/100,000, down from 52.6/100,000 in 1952. In DC, however, the rate is much higher, most recently 12-15/100,000 in 1999-2000. (I was unable to find more current data.) If you exclude the Northwest quadrant of the city, that rate would clearly be much higher yet. Considering that we do have pockets of high TB incidence like DC in the U.S., switching to a European-style policy of offering vaccination to high risk children may make good sense.
(Source: CDC)
An Aussie Idea
A recent paper in the Medical Journal of Australia suggested offering BCG vaccination to Australian medical students. They noted that although the Australian incidence of TB is low, Australian medical students like to perform foreign electives in areas of high TB prevalence, where having been vaccinated would benefit them.
A Few Conclusions
BCG isn’t a great vaccine, but it does provide an intermediate level of protection against TB, and it appears to be about equally effective as the treatment of latent disease once somebody has been infected. In this new era of serum interferon gamma, although cost may be an issue, TST interference is no longer a reason to withhold vaccination. BCG vaccination status matters, and we no longer need to treat our BCG vaccinated patients with positive TSTs if their interferon gamma is negative. As for the rest of the U.S. policy, it may be time for some revision.
Adapting a European-style vaccination model of offering vaccination to those children at highest risk for TB could selectively protect the children who need it without compromising our current methods of diagnosis, treatment, control, and prevention.
References (direct links provided to the others):
1Glassroth, Jeffrey and Christopher Crnich. Tuberculosis in Baum’s Textbook of Pulmonary Diseases. 7th ed. Lippincott Williams and Wilkins:2004.
2Criteria for discontinuation of vaccination programmes using Bacille Calmette-Guérin (BCG) in countries with a low prevalence of tuberculosis. A statement of the International Union Against Tuberculosis and Lung Disease. Tuber Lung Dis 1994;75(3):179-80